Jevaughn Davis MD1*, Caitlyn Stewart2, Haianha Desamour MD 1, Eric Heinz MD PhD3, Anita Vincent MD3
1AResident Physician, Department of Anesthesiology and Critical Care, George Washington School of Medicine and Health Sciences, Washington DC, USA
2Medical Student, George Washington School of Medicine and Health Sciences, Washington DC
3Attending Physician, Assistant Professor, Department of Anesthesiology and Critical Care, George Washington School of Medicine and Health Sciences, Washington DC 20037
*Corresponding author
Jevaughn Davis, MD Resident Physician, Department of Anesthesiology and Critical Care, George Washington School of Medicine and Health Sciences, Washington DC, USA
Abstract
Large goiters have been known to cause tracheal deviation or compression, presenting the potential for a difficult airway. If time allows, preoperative workup including multispecialty evaluation and advanced imaging can mitigate the potential for airway complications. Awake fiberoptic intubation is often the method of choice for the anticipated difficult airway but may not always be tolerable for patients. We herein describe a patient with a 10–15-year history of a large multinodular goiter causing tracheal deviation without overt symptoms of airway compression. Planned awake fiberoptic intubation was not tolerated by the patient due to opposition from the tongue and failure of scope advancement beyond the base of the tongue. The patient was later successfully intubated with video laryngoscopy after mask induction.
Keywords: Airway Management, Goiter, Difficult Intubations, Awake Fiberoptic Intubations, Video Laryngoscopy.
Introduction
A goiter describes an enlarged thyroid gland which can cause tracheal deviation or stenosis when sufficiently large [1], presenting significant difficulty in airway management. Careful consideration and planning must be given to the patient with a large goiter and should include thorough history and physical exam [2], multidisciplinary preoperative evaluation, and imaging, if time allows. Awake fiberoptic intubation (AFOI) is considered the gold standard for the anticipated difficult airway, though video laryngoscopy, amongst other techniques, can be used in combination with or instead of AFOI, with similar success rates [3-5]. Studies have shown that success of AFOI is largely dependent on the anesthesiologist’s familiarity with these techniques [3].
Aside from operator comfort with the chosen intubation method, appropriate sedation and analgesia are paramount to a successful AFOI [4, 6]. Sedation should be light enough to allow for spontaneous ventilation, as heavy sedation can lead to respiratory distress, apnea, or hemodynamic instability [7] while anxiolysis by medication or cognitive reassurance is integral. Analgesia can be delivered via topical anesthesia to the upper airway or by regional techniques to subdue cough and gag reflexes for decreased overall patient discomfort [4]. Unbalanced or incomplete sedation or analgesia can lead to treatment failure and contingency plans should be in place if AFOI is not successful.
We present the case of a patient with a large goiter presenting without respiratory distress or upper airway complaints, who underwent rigorous preoperative imaging and multispecialty evaluation. AFOI was planned and attempted but was unsuccessful due to patient intolerance. The patient was successfully intubated with video laryngoscopy after mask induction with sevoflurane.
Case Presentation
An 82-year-old (53kg) woman with a 10–15-year history of goiter presented for one day duration of right leg pain after a mechanical fall 3 months prior. She was initially mobile without issues until her pain acutely increased the prior day. Her emergency room work up was notable for an acute femur fracture. Labs were notable for elevated white blood cell count of 15.83, and findings consistent with subclinical hyperthyroidism, which included elevated thyroid stimulating hormone (TSH), free thyroxine (FT4) and free triiodothyronine. She reported having an intermittently rapid and irregular heartbeat, increased anxiety and nervousness and dysphagia to solids initially. She adapted for her dysphagia by eating slower, taking smaller bites, and chewing her food well. Otherwise, she denied issues with respiration and had noticed no changes in her respiratory patterns in the last 5 years. Vitals were notable for a respiratory rate of 34 and a heart rate of 110 for which her primary team started her on propranolol. Physical exam was notable for a visible, and mobile goiter (Figure 1). She had no known allergies and was not taking any medications. Family history was noncontributory. There was no familial or personal history of complications with anesthesia, and no prior intubations. Surgical history was pertinent for a prior cesarean section. American Society of Anesthesiologists (ASA) physical exam score was IV.
Figure 1: Neck Goiter.
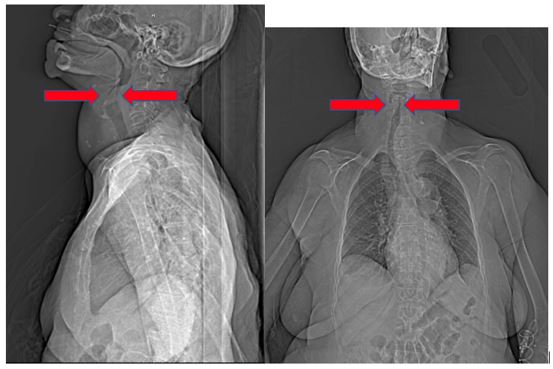
Admission two view chest x-ray was notable for tracheal deviation and subglottic narrowing (Figure 2A/B). The anesthesia team peri-operatively evaluated her, wherein she was a mallampati class II and she denied respiratory symptoms or trouble with lying flat. Beside ultrasound revealed a vascular mass with a patent trachea while upright and moderate compression when the head of the bed was less than 30 degrees. Trauma surgery was consulted for a surgical airway should intubation attempts prove unsuccessful. Trauma surgery determined the borders of the mass were unclear and expressed concerns that if intubation failed and urgent surgical exploration needed, a surgical airway would be challenging and potentially unsuccessful given the unknown anatomy. They determined the mass to be hypervascular, and a surgical airway could lead to massive hemorrhage. The case was moved to another day for a more robust evaluation of the neck mass.
Figure 2: Tracheal deviation to right and airway compression. A: Chest x-ray, left lateral view. B: Chest x-ray, frontal view.
Ultrasound revealed a markedly enlarged thyroid gland compatible with a goiter containing multiple enlarged nodules with two right nodules measuring 5.2 x 4 x 5 cm and 5.2 x 4 x 4.2 cm in addition to a left nodule measuring 5.6 x 4.6 x 5.2 cm. The thyroid was enlarged and heterogeneous with multiple coarse calcifications with the left lobe measuring 11.4 x 6.3 x 7.9 cm and right lobe measuring 8.6 x 5.2 x 4.7 cm. All nodules were heterogeneous with solid, mixed solid, cystic, and calcified parts. A computerized tomography (CT) neck and soft tissue scan was performed and demonstrated an enlarged heterogeneous thyroid gland with multiple coarse calcifications with the left lobe greater than right lobe (Figure 3). The left lobe measures 11.4 x 6.3 x 7.9 cm and the right lobe measures 8.6 x 5.2 x 4.7 cm, with the largest nodule in the right gland measuring 6.0 x 4.0 x 4.7 cm the upper /mid pole (Figure 4A/B).
Figure 3: Computed tomography scan of the goiter.
Figure 4: Computed tomography soft tissue scan demonstrating the Right and Left nodules of the goiter. A: Coronal cross-sectional view. B: Sagittal cross-sectional view.
On CT neck and soft tissue, the airway proved to be largely patent with regions of luminal narrowing (Figure 5). Otorhinolaryngology performed a flexible fiberoptic laryngoscopy and discovered a widely patent airway without significant airway compression. Both trauma surgery and otorhinolaryngology surgery opted to be available for intubation.
Figure 5: Computed tomography neck and soft tissue scan demonstrating the airway. Sagittal view, red arrow represents the area of mild narrowing.
The decision was made to perform an awake fiberoptic intubation for patient safety in the setting of a possible difficult intubation. Induction began with 0.4 mg IV glycopyrrolate and nebulized 5% lidocaine in the preoperative area for 30 minutes. The patient was then taken to the operating room, where she was placed on standard monitors in addition to nasal cannula with capnography. A remifentanil infusion was started at 0.07mcg/kg/min and topical 4% lidocaine gel was administered bilaterally to the tonsillar pillars. After about seven minutes, the fiberoptic scope was introduced; however, despite the absence of a gag or cough reflex, the scope could not be advanced without the patient’s tongue actively fighting provider efforts. A second attempt was made with jaw lift and tongue retraction, however the patient’s tongue continued to interfere with fiberoptic scope advancement. The decision was made to abandon awake fiberoptic intubation since the patient was easily masked. Anesthesia was induced with 8% sevoflurane in oxygen with the patient in a semi-recumbent position and anesthesia was maintained with 50% oxygen and sevoflurane for a minimum alveolar concentration of 1.2 after intubation. A 7.0 reinforced endotracheal tube was inserted with the aid of a C-MAC video laryngoscope after obtaining a grade 2 Cormack and Lehane view. After confirmation of placement with end-tidal carbon dioxide, paralytic was administered (30 mg IV Rocuronium) for the surgical procedure. Additionally, the patient was given 10 mg IV Dexamethasone, 4 mg IV Ondansetron, 40 mg IV Ketamine, 2g IV Ancef, and 0.7 mg IV Hydromorphone during the case. Neuromuscular train-of-four ratio was continuously monitored and at the end of the case, the patient was reversed with 200 mg IV Sugammadex and a train-of-four with height greater than 0.9 was obtained. After full inhalational agent washout, the patient met extubation criteria and was extubated to nasal cannula without issues. In the post anesthesia care unit (PACU), she was maintained on nasal cannula with capnography in the event additional IV opioids were needed for operative pain. A fascia iliaca nerve block was placed for further pain control to minimize opioid usage. PACU stay was uneventful, and she returned to her inpatient room.
Discussion
Goiters can often be accompanied by airway deformities leading to difficult or challenging mask ventilation and or laryngoscopy. Induction of anesthesia in these cases can lead to complete airway closure, making mask ventilation and tracheal intubation difficult, leading to unintended surgical airways or cardiopulmonary mortality and morbidity [8-9]. Cardiorespiratory complications occur approximately 14.3% [8] of the time in patients with anterior or middle mediastinal masses. Cardiorespiratory signs and symptoms at the time of presentation usually confer the highest rates of perioperative complications [8-9]. Partial or complete airway closure is usually in part due to the pressure exerted on the trachea by surrounding soft tissue especially during periods of tissue relaxation such as during sleep, sedation and under general anesthesia. Induction of anesthesia can result in increased relaxation of soft tissues which causes the soft tissue to collapse onto the surrounding airway, increasing the pressure being exerted on the trachea. This mass effect on the trachea can be alleviated or worsened in certain positions due to gravity. It is often important to probe patient history about “how they sleep” or whether being supine causes any respiratory issues. Ideally these patients should be preoxygenated and intubated in the position most comfortable to them. This is the position least likely to cause respiratory symptoms, panic and is most likely to avoid tracheal compression.
Many techniques can be used to aid intubation in this population. Ideally, spontaneous respiration should be maintained. Spontaneous respirations preserve negative pleural pressure, which allows for patency of the airway. Thus, sedation should be minimized, or providers should use sedative agents that minimally affect respiratory function and tone. These agents include ketamine, dexmedetomidine and ultra-low doses of remifentanil. When possible general anesthesia should be substituted for neuraxial or regional anesthetic techniques as these techniques offer lower potential for respiratory depression, apnea and or loss of airway.
Depending on anesthesiologist preference, techniques such as awake direct laryngoscopy, awake tracheostomy, awake fiberoptic intubation or awake rigid bronchoscopy may be utilized. Awake fiberoptic intubation has won favor with many anesthesiologists given its versatility and its ability to allow continuous ventilation if placed through a laryngeal mask airway. There is no significant difference in the first attempt success rates of fiberoptic intubation and video laryngoscopy [3]. Alhomary et al. found that intubation times were shorter for video laryngoscopy and there were no significant differences in failure rates [3]. There was no difference when comparing adverse events like postoperative hoarseness, sore throat, or low oxygen saturation [3]. In this case, awake fiberoptic intubation was unsuccessful while mask induction with sevoflurane and video laryngoscopy led to a successful outcome. Based on the current literature, video laryngoscopy and awake fiberoptic are both effective and comparable techniques, thus depending on the clinical scenario, fiberoptic intubation should not be the automatic default technique and thought and consideration should be given to video laryngoscopy or awake laryngoscopy. The competency, skill set, and experience needed by anesthesiologists for video laryngoscopy and fiberoptic are different. It is estimated that an anesthesiology needs to perform 25 fiberoptic intubations to become competent when compared only 6 video laryngoscopes for competency [10].
Conclusion
Goiters when large enough present an increased risk of cardiopulmonary complications surrounding management. For non-emergent surgeries, patients should be properly optimized. Optimization involves up to date imaging and identification of the goiter and its effect on the patient’s underlying airway. Comprehensive planning involves a multidisciplinary medical team, proper preoperative assessment, and discussion to best provide a safe outcome for the patient. Video laryngoscopy and awake fiberoptic are both effective and comparable techniques. Both techniques should be considered depending on the clinical scenario.
Disclosures: None
Acknowledgements: This case report was written and published with the written consent of the patient.
Conflict of Interest: There is no external funding or competing interests to be declared.
REFERENCES
- Can AS, Nagalli S. Substernal Goiter. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 4, 2022.
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251-270. doi:10.1097/ALN.0b013e31827773b2
- Alhomary M, Ramadan E, Curran E, et al. Videolaryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation: a systematic review and meta-analysis. Anaesthesia. 2018;73(9):1151-1161. doi:10.1111/anae.14299
- Cabrini L, Baiardo Redaelli M, Ball L, et al. Awake Fiberoptic Intubation Protocols in the Operating Room for Anticipated Difficult Airway: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Anesth Analg. 2019;128(5):971-980. doi:10.1213/ANE.0000000000004087
- Collins SR, Blank RS. Fiberoptic intubation: an overview and update. Respir Care. 2014;59(6):865-880. doi:10.4187/respcare.03012
- Langeron O, Bourgain JL, Francon D, et al. Difficult intubation and extubation in adult anaesthesia. Anaesth Crit Care Pain Med. 2018;37(6):639-651. doi:10.1016/j.accpm.2018.03.013
- Tang ZH, Chen Q, Wang X, et al. A systematic review and meta-analysis of the safety and efficacy of remifentanil and dexmedetomidine for awake fiberoptic endoscope intubation. Medicine (Baltimore). 2021;100(14):e25324. doi:10.1097/MD.0000000000025324
- Srivastava D, Dhiraaj S. Airway management of a difficult airway due to prolonged enlarged goiter using loco-sedative technique. Saudi J Anaesth. 2013 Jan;7(1):86-9. doi: 10.4103/1658-354X.109829.
- Tan PC, Esa N. Anesthesia for massive retrosternal goiter with severe intrathoracic tracheal narrowing: the challenges imposed -A case report-. Korean J Anesthesiol. 2012 May;62(5):474-8. doi: 10.4097/kjae.2012.62.5.474
- Moore A, Schricker T. Awake videolaryngoscopy versus fiberoptic bronchoscopy. Current Opinion in Anaesthesiology. 2019;32(6):764–8.