Mechanical support in cardiogenic shock after synchronised electrical cardioversion
Vittorakis Eftychios*, Sinanis Theodoris
Department of Cardiology and Cardiology intensive care unit, Agios Georgios, General hospital of Chania, Chania, Greece.
*Corresponding author
*Vittorakis Eftychios, Department of Cardiology and Cardiology intensive care unit, Agios Georgios, General hospital of Chania, Chania, Greece.
DOI: 10.55920/JCRMHS.2023.04.001172
Case Study
A 53-year-old male patient presented to our emergency department with a worsening dyspnea that had reached clinical status new York heart association (NYHA) level III to IV. The patient had been hospitalized for approximately one week, three months prior, in the neurology department due to a minor stroke that left no current deficit. During this hospitalization, a newly diagnosed atrial fibrillation was found to be the cause of the stroke, and oral anticoagulation was initiated after a few days. At that time, a transthoracic echocardiogram showed a normal left ventricular ejection fraction with no moderate or severe structural or functional valvulopathies.
At the time of the current presentation, the patient was still experiencing atrial fibrillation, and reported excessive alcohol and cigarette consumption. Clinical examination revealed signs of congestive heart failure, and intravenous diuretics were initiated. A new transthoracic echocardiogram showed a severe limitation of the left ventricular pump function with the ejection fraction now around 20%. As tachycardia-induced cardiomyopathy was considered a differential diagnosis, synchronized electrical cardioversion was performed after three days of hospitalization. A total of 6 ml of Propofol 1% was used for sedation, and the cardioversion was successful in achieving sinus rhythm.
During the recovery phase, while still being monitored, the patient went rapidly into shock and developed pulseless electrical activity. A reanimation protocol was initiated, which was successful after approximately 10 minutes. The patient remained intubated and required high doses of inotropes (dobutamine and noradrenaline) for a few hours with no diuresis, when a new worsening of the blood pressure began. At that point, an intra-aortic balloon pump (IABP) was inserted through the left femoral artery. After that, the dose of inotropes could be slowly reduced, and after 72 hours, the patient required no inotropic support anymore. Due to a lung infection treated with tazobactam, the patient remained intubated for four more days, and at day 7 of his stay in the intensive care unit, he could be extubated.
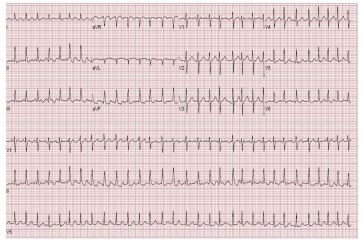
Figure 1: Electrocardiography with Atrial Fibrillation.
Figure 2: Chest radiograph of the patient exhibiting an augmented intrathoracic diameter while utilizing an intra-aortic balloon pump.
Figure 3: Intra-aortic balloon pump (IABP).
During the rest of his hospital stay, the patient developed atrial fibrillation once more, and amiodarone therapy was initiated. A new transthoracic echocardiogram in sinus rhythm showed an ejection fraction of 20%. A coronary angiogram was also performed, and coronary heart disease could be excluded. At day 19 of his hospital stay, the patient was discharged.
Discussion
This is a case report detailing a rare complication of a generally safe medical procedure. Although pulseless electrical activity due to Takotsubo syndrome resulting from electrical cardioversion has been previously documented, it was not observed in this particular patient. This case report highlights the necessity of intraaortic balloon pump (IABP) treatment for cardiogenic shock following electrical cardioversion, and suggests that IABP may confer a clear mortality benefit in hospitals where Impella or ECHMO are not available.
Regarding this case, while tachycardia-induced cardiomyopathy cannot be ruled out, alcohol-induced cardiomyopathy is also a possible explanation for the low ejection fraction. In hindsight, a more aggressive therapy with diuretics and optimization of heart failure treatment prior to the electrical cardioversion may have prevented the occurrence of pulseless electrical activity. Furthermore, the patient's deteriorating status could be attributed to sedation, as both cardiac arrest and cardiogenic shock after propofol administration have been reported in the literature [5].
- Hindricks, G., Potpara, T., Dagres, et all; ESC Scientific Document Group. (2021). 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. European Heart Journal, 42(5), 373-498. doi: 10.1093/ eurheartj/ehaa612.
- Grönberg T., Nuotio I., Nikkinen et all; (2013). Arrhythmic complications after electrical cardioversion of acute atrial fibrillation: the FinCV study. Europace, 15(10), 1432-1435. doi: 10.1093/europace/eut106.
- Nusair, M., Flaker, G. C., & Chockalingam, A. (2010). Electric cardioversion of atrial fibrillation. Missouri Medicine, 107(1), 59-64.
- Landi, A., & De Servi, S. (2021). Takotsubo syndrome and electrical storm following electrical cardioversion of atrial fibrillation: cause, consequence or both? Journal of Cardiovascular Medicine (Hagerstown), 22(2), 139-142. doi: 10.2459/ JCM.0000000000001021.
- Renilla González, A., Lozano Martinez-Luengas, I., Benito Martín, E. M., et all; (2011). Cardiogenic shock following administration of propofol and fentanyl in a healthy woman: a case report. Journal of Medical Case Reports, 5, 382. doi: 10.1186/1752-1947-5-382.