Zulay Palima González1, Miccelis Escalante2, Heriberto López3, Ligia Pérez4
1UNERG dentist, UNERG teacher, dental school, applied biochemistry subject, specialist in UNERG university teaching, master's degree in oral surgeon CIU and DRA. in educational sciences UPEL
2UC dentist, graduate in oral surgery I,II,III,IV.
3UC. dentiste,Oral and Maxillofacial Surgeon UC. Ordinary teacher of undergraduate oral surgery UC. Postgraduate teacher of oral and maxillofacial surgery, orthodontics, endodontics and odontopediatrics UC. Director and creator of specialization in oral surgery ULC
4LUZ dentist, bucomaxillofacial pathologist, Dr. in Dentistry, Full Professor of Pathology II, LUZ, Fellow of the American Academy of Oral and Maxillofacial Pathology, Professor of Pathology at Larkin Hospital in Miami.
*Corresponding author
*Zulay Palima González, UNERG dentist, UNERG teacher, dental school, applied biochemistry subject, specialist in UNERG university teaching, master's degree in oral surgeon CIU and DRA. in educational sciences UPEL
Abstract
Introduction: Slow and painless growth pathologies such as (TOA) depend on the interest of the patient to attend on time or at the wrong time to know what happens with this increase in volume in their oral cavity, in the case presented below, It was when he affected the aesthetics that he decided that it merits solving what he is presenting and taking into account that it is benign, it can have a recurrence, for that reason the appropriate treatment and controls are of great importance.
Objectives: General objective; To analyze the surgical approach applied to a 19-year-old female patient who presents with Adenomatoid Odontogenic Tumor; and among its specific objectives is: Identify the clinical and radiographic manifestations present in a 19-year-old female patient. In the theoretical review, reference was made to aspects such as: origin of the adenomatoid odontogenic tumor, histology, treatment, differential diagnosis, among others.
The methodology: Used corresponds to the modality of a descriptive project under a positivist paradigm being field since the data were collected directly in the reality where the events occurred. The population and sample is made up of a 19-year-old female patient.
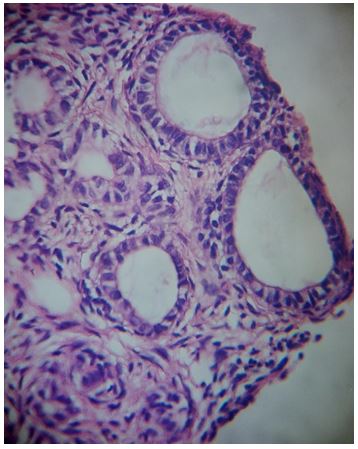
Results: Performed an enucleation and excision of the lesion with a subsequent histopathological study of the same that confirmed the possible clinical diagnosis.
Conclusions: Any increase in volume, change in color and texture, must be evaluated through your clinical history, complementary examinations, photographic records and histopathological study, which indicates an accurate diagnosis and treatment, the (TOA) also indicates clinical, radiological and warrant follow-up. Histopathological, if any recurrence occurs.
Key Words: Tumor, Odontogenic, diagnostic, adenomatoid, histopathological, adenomatoid.
INTRODUCTION
One of the innumerable pathologies that frequents oral surgery is the adenomatoid odontogenic tumor, (TOA) a tumor that over the years has been studied and carried with it different theories about its origin and names. TOA is a benign, slow-growing neoplasm that can be observed clinically as an increase in volume both extra and intraorally, it is asymptomatic and non-invasive. This same has been classified by the World Health Organization (2017) as an epithelial odontogenic tumor with a varied histoarchitectural pattern of a mature fibrous stroma without odontogenic ectomesenchyme, with structures and with induction in the connective tissue of variable degree1.
As previously mentioned, there are controversies regarding the origin of the TOA, however, this tumor could originate in an area where the teeth are formed, since it presents several components of the enamel organ, the dental lamina and the reduced epithelium. of the enamel.
Development
The Adenomatoid Odontogenic Tumor is a lesion classified by the WHO (2017) within the odontogenic tumors with the participation of the ectomesenchyme, since it may contain, in addition to the epithelium, calcified tissue inside; It is a slow-growing and minimally invasive lesion, but it can be similar to other more aggressive odontogenic lesions such as the dentigerous cyst and ameloblastoma, among others.
Its classic location (upper canine area) guides us to the diagnosis and its ductiform histological pattern is very typical of this tumor. The adenomatoid odontogenic tumor (AOT) is a rare, benign, non-invasive, slow-growing and progressive tumor, which represents 3% of odontogenic tumors. Due to the slow-growing and asymptomatic nature of the tumor, it may present an increase in volume to produce visible facial deformities, often causing tooth displacement, and in some cases root resorption 2-3.
Likewise, the adenomatoid odontogenic tumor presents variations depending on the site of origin or appearance thereof. There are two clinical variants: intraosseous (97.7%) and extraosseous (2.3%). Intraosseous is subdivided into: a) Pericoronal or follicular (70.8%) and b) Extracoronal or extrafollicular (26.9%). When it occurs extraosseous, the predilection site is the lower anterior gingiva. Pericoronal intraosseous TOA is associated with an impacted tooth in which approximately 60% of cases is a canine, predominantly in the upper arch; Very rarely, permanent incisors, molars and premolars, and even deciduous teeth may be involved. The extrafollicular type is also intraosseous, but is not associated with an impacted tooth.4
On the other hand, it is important to highlight the relevance of making an accurate diagnosis taking into account differential diagnoses since TOA tends to have similar characteristics to other odontogenic lesions, based on complementary examinations and special radiographs. In accordance with what was previously said, the patient must correctly answer all the questions asked by the operator, this whole series of questions is known as anamnesis, in this way it will guide us to correctly carry out the definitive diagnosis, these processes lead to the planning of an appropriate treatment plan for the patient.
Saldaña, M., Martins, V. de Albuquerque, G. & Júnior, J. (2020). Extrafollicular adenomatoid odontogenic tumor: case report. San Marcos Dentistry, 23(1), 51-55. The usual treatment of choice in all cysts is enucleation, which is nothing more than the complete removal of the lesion adhered to the bone in question, this with the reason that it allows the performance of a subsequent excisional biopsy for the pathological study of the cyst. injury5. Although the adenomatoid odontogenic cyst is a lesion with little recurrence, follow-up should be carried out after the surgical process itself to assess the status and evolution of the patient before the indicated treatment.
Presentation of the clinical case
CLINIC HISTORY, PERSONAL INFORMATION:
PATIENT:AGE: 19 Years; SEX: Female; Student occupation.
NATURAL: San Fernando de Apure, Apure State, Venezuela. ORIGIN: San Fernando de Apure, Apure State, Venezuela.
CLINICAL DATA
REASON FOR CONSULTATION: "Volume increase in the upper anterior area"
CURRENT DISEASE: This is a female patient of 19 years of natural age and from San Fernando de Apure, attends the dental office presenting an increase in volume in the upper right anterior area, since November 2019, slowly and progressively, which affects the region of the nasolabial fold, right wing of the nose, upper lip, with labial incompetence, associated with increased volume, does not report pain, only aesthetics bother him.
FAMILY HISTORY: the patient reports that his father, mother and grandparents are apparently healthy, with no underlying pathological history.
PERSONAL HISTORY: No underlying pathological history.
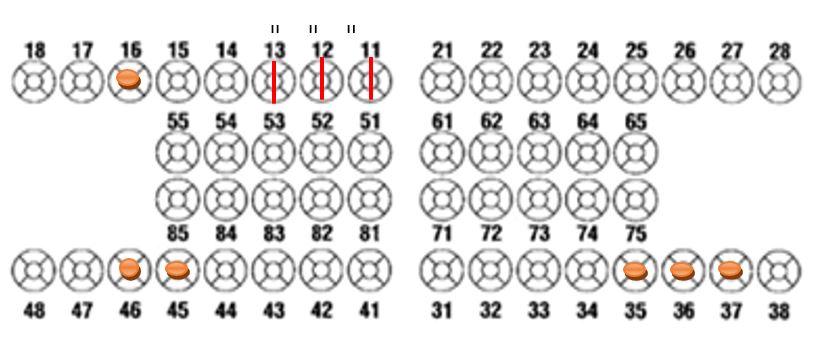
CLINICAL FINDINGS: soft tissue examination revealed intraoral edema in the upper right part, with volume increase from units: 11, 12 and 13, loss of normal characteristics of the gingiva, adjacent mucosa, and slight displacement of the units. : 12 and 13, on probing a sac greater than 11 mm, in units: 11, 12, and 13, presenting grade II mobility, on endodontic examination, positive vitality tests, in the pathological evaluation, a round lesion is described, of sessile, well encapsulated base of approximately 3cm X 3cm, where aspiration and excisional biopsy is suggested, on examination of the hard tissues there is loss of calcified substance in you: 16, 35, 36, 37, 45, 46, the patient does not present no type of habit.
Figure 1: ODONTODIAGRAM
RADIOLOGICAL EXAMINATION
The radiological examination shows a circumscribed radiolucent image, with regular edges of approximately 3cm X 3cm in the upper right anterior zone, where displacements of radiopaque structures compatible with ud are observed: 12 and 13, increased periodontal ligament space.
PRESUMPTIVE DIAGNOSIS
- Adenomatoid odontogenic tumor
- Dentigerous cyst
- Paradental cyst
- Unicystic ameloblastoma
DEFINITIVE DIAGNOSIS
- Adenomatoid odontogenic tumor.
HISTOPATHOLOGICAL DIAGNOSIS
- Adenomatoid odontogenic tumor, with atypical cells, with possible recurrence
FORECAST
- General: It is good because the patient does not have any systemic disease that compromises the treatment.
- Individual for UD 11,12,13 reserved, possible root canals or extractions, depending on the evolution of the patient.
TREATMENT PLAN
Initial phase
- Performance of orthopantomography
- Performance of cone beam tomography
- Taking photographic records
- Case planning
surgical phase
- Enucleation of the lesion
- Sampling for biopsy
maintenance phase
- Postoperative evaluation at 8 days and later at 21 days.
- Histopathological results.
- Assessment at 2 months
- Photographic record.
APPROACH TO THE CASE
Quote 1:
We proceed to fill out the clinical history, clinical review, orthopantomography assessment, given the finding, the clinical signs and symptoms present, CT is indicated, laboratory tests, extra and intraoral photography, for the analysis and presentation of the clinical case.
Figure 2: Images, Extra oral source. Source Palima and Escalante, M. (2019) Image: (a) forehead (b) smile forehead (c) right profile (d) left profile (e) profile right at 45° (f) left profile 45°.
Figure 3: Intraoral Images Fuente Palima,z. and Escalante, M. (2019) Image (a) front (b) right profile (c) left profile
Figure 4: Intraoral Images. Fuente Palima, Z. and Escalante, M. (2019) Image (a) Upper occlusal (b) Lower occlusal (c) Occlusal profile.
Intraoral photographs are of great help for the diagnosis of pathologies in patients, they are a useful and additional tool that provides valuable information for the dental professional, it provides clinical records, in this case oral surgery.
Appointment 2
We proceed to evaluate and analyze the initial orthopantomography, in which a lesion of approximately 3 cm is evidenced since this is referential, evaluation of CT images, analysis of the imaging report and laboratory tests, already with all these clinical and imaging data, We proceed to the discussion and surgical planning in which it is decided to perform an enucleation of the lesion and subsequently perform a histopathological study.
Figure 5: X-rays and cone beam tomography Fuente Palima, Z and Escalante, M. (2019). Image (a) orthopantomography (b) right lateral view and palatal view, cone beam tomography.
Figure 6: Cone beam tomography. Source Palima, Z. and Escalante, M. (2019). Images palima,z. 2020).Image (a) frontal and occlusal view (b) transaxial slices of cone beam tomography showing size and how much the dental organs are involved with a well-defined hypodense image.
Figure 7: Cone beam tomography. Fuente Palima, M. and Escalante, M.(2019).images palima,Z.(2019).Images (a) hypodense and hyperdense images that guide the magnitude and volume of the lesion (b) axial slices of the maxillary area, with images hypodense and hyperdense that guide surgical planning.
Appointment 3
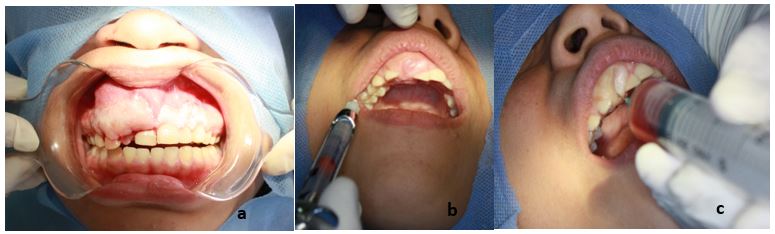
Informed consent was obtained in which the surgical procedure, the risks and possible complications are explained to the patient, the patient signs and places both thumb prints, and the surgical act itself is subsequently carried out.
It is decided to carry out the enucleation and excision of the entire lesion for the histopathological study of excisional biopsy, beginning with the asepsis and antisepsis of the patient, proceed to the application of anesthetic with 2% lidocaine and articaine to reinforce the operating time, in third In this step, the Newman type incision and flap is made from the lateral incisor on the adjacent side to the premolars on the right side.
Figure 8: Intraoral images surgical phase. Fuente Palima, z and Lopez, H. Escalante, M. (2019). Images (a) front (b) infiltrative anesthesia with 2% lidocaine 1:100,000 epinephrine V2, V. middle Anterior (c) positive aspiration of content 6 CC
Figure 9: Images Surgical phase. Source Palima, z. and Lopez, H. Escalante, M. (2019) Image (a) after aspiration for size reduction (b) Newman incision
Figure 10: Images Source Palima, Z. and Lopez, H. Escalante, M. (2019) Image (a) lifting of trapezoidal flap (b) enucleation itself (c) total removal (e) single stitch suture (f) finished suture.
Once the treatment is finished, the indications and post-operative care are explained to the patient, where the following is indicated:
1.-Consumption of a soft and cold diet for 8 days
2.-Bite the gauze for 1 hour
3.-You must have a correct and normal oral hygiene of the area and mouth in general
4.-Do not perform physical activity that generates the application of excessive force
5.-Place cold compresses at intervals of 3-5 min, resting and repeating 6.-as many times as necessary for 24 hours
7.-It is recommended to avoid dairy consumption
8.-Application of rinses with chlorhexidine for 8 days
9.-The analgesic of choice was ibuprofen 400 mg every 8 hours for 3-5 days, amoxicillin 500 mg every 8 hours for 7 days and 1 dexamethasone in a vial, single dose.
In addition to these general care, the patient is told that dental units 11, 12 and 13 require endodontics since the vascular and nervous part was compromised in the surgical act itself and a possible pulp necrosis is not ruled out in time.
Figure 11: Postoperative. Source Palima, Z. López, H. Escalante, M (2020). Post-operative control image 3 months after surgery, the teeth maintain vitality and do not present mobility, gums with hyperplasia are observed, displacement of ud:12.
Figure 12: Histological slide source Pérez, L. (2019)
CONCLUSIONS AND RECOMMENDATIONS
According to the specific objective No. 1, the 19-year-old female patient who presents an adenomatoid odontogenic tumor goes to the dental office where an increase in volume in the upper anterior sector is evidenced in its clinical manifestations, with the presence of mobility. dental units: 11, 12, 13. On radiographic examination, a widening of the periodontal ligament can be observed, as well as a displacement of the roots of the dental units: 12, 13.
In response to specific objective No. 2 after the clinical observation of the 19-year-old female patient, she was instructed to undergo laboratory tests, panoramic radiography, and computed tomography.
The surgical procedures applied to a 19-year-old female patient who attended the dental office due to increased volume in the upper anterior area, concluding that the pathology present is an adenomatoid odontogenic tumor, based on the treatment indicated step by step. step in this case is carried out, informed consent, planning, asepsis and antisepsis of the area with surgical isolation, application of anesthesia using the technique: infiltration of the median and anterior alveolar nerve, then proceed to perform the surgical act itself in the following order Neumann incision or trapezoidal flap, aspiration using a 20cc syringe, complete enucleation of the lesion for a subsequent excisional biopsy, curettage, slight osteotomy to eliminate possible affected tissues and application of suture, photographic record.
Lastly, in response to specific objective No. 4, general care was established: a soft liquid and cold diet for 8 days, biting the gauze for 1 hour, normal hygiene of the area and mouth in general, placing cold compresses at intervals. 3-5 min, resting and repeating as many times as necessary for 24 hours, avoid dairy consumption for 3 days, to avoid fermentation around the suture, rinse with chlorhexidine for 8 days, ibuprofen-type analgesic 400 mg every 8 hours for 3-5 days, amoxicillin 500 mg every 8 hours for 7 days, 1 dexamethasone in vial, single dose.
CONCLUSIONS
Before carrying out any surgical treatment itself, a correct diagnosis must be made accurately based on an anamnesis, complementary studies and differential diagnoses in order to correctly generate an appropriate treatment plan for each patient. In addition to this, the operator in charge must explain the entire treatment plan in detail in order to generate confidence and peace of mind for the patient.
The dental professional, in this case the treating oral surgeon, must rigorously follow all the steps before a surgical procedure, without leaving aside the prior asepsis and antisepsis of the patient, operator and the instruments to be used. In addition, all those possible complications that could be generated in the application of the surgical treatment itself should be known.
After the surgical procedure, post-operative check-ups are recommended after 8 and 21 days and later evaluation at 2 months to evaluate the case in question since, although there are low recurrence rates, each case must be closely evaluated.
It is recommended that dental professionals continue to deepen the subject, as well as make contributions of cases of adenomatoid odontogenic tumor. In this sense, it is recommended that the authorities of the "Rómulo Gallegos" National Experimental University (dentistry area), and the professors of the surgery area, include in the training of students how to approach such cases.
REFERENCES
- OMS (2017) Clasificación de los tumores odontogénicos: evolución y cambios citado por,Dra. Vanesa Pereira Prado https://www.dnsffaa.gub.uy/media/images/41a46-clasificacion-de-los.pdf?timestamp=20180808113327.
- Marín Botero, ML, Sáenz Rivera, E de J, Marín Cardona, MN, Sánchez Muñoz, LB, & Castañeda-Peláez, DA. (2017). Tumor odontogénico adenomatoide. Reporte de un caso y revisión de la literatura. Avances en Odontoestomatología, 33(4), 161-170. Recuperado en 01 de noviembre de 2021, de http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0213-12852017000400004&lng=es&tlng=es.
- Mosavat F, Rashtchian R, Zeini N, Goodarzi Pour D, Mohammed Charlie S, Mahdavi N. An extrafolli-cular adenomatoid odontogenic tumor mimicking a periapical cyst. Case Rep Radiol. 2018. https://doi.org/10.1155/2018/6987050.
- Bhandari N, Kothari M. Adenomatoid odontogenic tu-mour mimicking a periapical cyst in pregnant woman. Singapore Dent J.2010;31(1):26-9.
- Saldaña, M. A. Q., de Oliveira, M. V., Martins, V. B., de Albuquerque, G. C., & Júnior, J. M. (2020). Tumor odontogénico adenomatoide extrafolicular: reporte de caso. Odontología sanmarquina, 23(1), 51-55.