Anterior Subtenon Cyst Formation after Triamcinolone Injection during Ahmed Glaucoma Valve Implantation: A Case Report
Naveed Nilforushan1, Farhad Najafzadeh2*
1Professor of Ophthalmology, Rassoul Akram Hospital, Iran University of Medical Sciences, Tehran, Iran.
2Assistant of Ophthalmology, Nikookari Eye Hospital, Tabriz University of Medical Sciences, Tabriz, Iran.
*Corresponding author
Farhad Najafzadeh, Assistant of Ophthalmology, Nikookari Eye Hospital, Tabriz University of Medical
Sciences, Tabriz, Iran.
DOI: 10.55920/JCRMHS.2023.04.001170
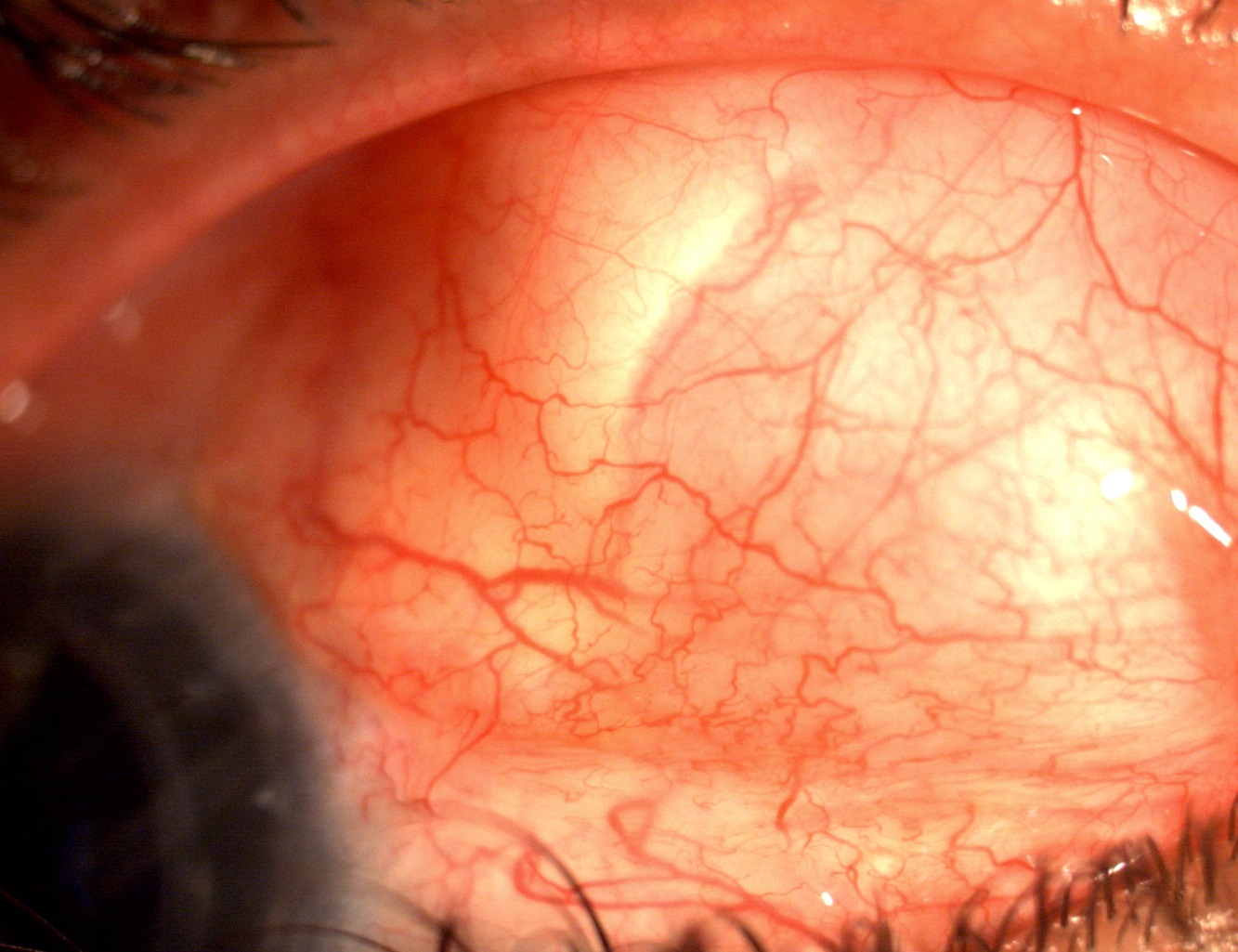
Figure 1: A 54-year-old male with previous history of penetrating keratoplasty who developed an anterior tenon cyst 3 weeks after AGV implantation with triamcinolone injection
Case 2:
The patient was a 43-year-old male diagnosed with Fuchs Heterochromic Iridocyclitis and glaucoma who underwent AGV implantation with triamcinolone injection. An anteriorly located thin-walled subtenon cyst formation with picture and symptoms similar to case 1 was detected 3 weeks after the surgery (Fig. 2). IOP was 16 at the time of cyst formation. The approach was similar to case 1, with multiple needling sessions, and a complete improvement of the cyst after 11 months. Also, IOP decreased significantly after each needling; the IOP was 14 mmHg at the last follow-up with a fixed combination eye drop of Timolol/ Dorzolamide. No complications were detected after each needling.
Figure 2: A 43-year-old male with diagnosis of Fuchs Heterochromic Iridocyclitis who developed an anterior thin walled tenon cyst 3 weeks after AGV implantation with triamcinolone injection
A 43-year-old male with diagnosis of Fuchs Heterochromic Iridocyclitis who developed an anterior thin walled tenon cyst 3 weeks after AGV implantation with triamcinolone injection
Case 3:
A 7-year-old child diagnosed with Aphakic glaucoma underwent AGV implantation with the same method of subtenon triamcinolone injection during surgery. Two weeks after surgery, an anterior thin-walled cyst with temporal conjunctival bulging and exposure was detected, involving patient discomfort and parental concern. IOP was 20 at the time of cyst formation. The cyst gradually decreased after 2 needling sessions performed over 8 weeks with no complications. After 6 months, there were no obvious cystic changes at the plate site, with no conjunctival exposure or patient discomfort. After each needling, IOP decreased significantly, and 1 year after surgery, the IOP was 14 mmHg with Timolol drops once a day.